The nose is one of those body parts that haunts half of the human population. Especially after it became possible to make adjustments to natural data. If there is a fashionable trend for plastic surgery, then rhinoplasty - correction of the shape of the nose - may well top the top. Plastic surgery clinics compete with each other for patients, attracting attention with colorful photos of the owners, often the owners, of new graceful noses. The desire to correct this particular part of the body is understandable: the nose “sets the tone” for all facial features. Sometimes the “before” and “after” photos are amazing – there are so many different faces looking at you. But is it always necessary to chase changing fashion? Should we expect miracles from plastic surgery? We will discuss these and other pressing issues with Aram Grigoryan .
The essence and types of rhinoplasty
Rhinoplasty can be performed for both aesthetic and functional reasons.
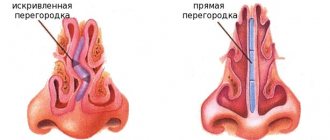
- Combining nasal reshaping with septoplasty can effectively treat certain breathing problems.
- Rhinoseptoplasty is also a reconstructive surgery aimed at correcting a birth defect or injury, such as a broken nose.
- It is performed under intravenous sedation or general anesthesia.
Story
The first attempts at Rhinoplasty date back to ancient times. At first, they boiled down to covering the gaping opening of the nose with tissue adjacent to the defect. Such an intervention only eliminated the repulsive impression of the exposed nasal cavity, but the resulting flat shape of the face could not satisfy either the patients or the surgeons.
Rice. 1. Stage of the Indian method of rhinoplasty: a flap of skin on a feeding pedicle is cut out in the forehead area.
Attempts at Rhinoplasty using forehead tissue were made in India in ancient times. From the forehead, in the shape of a flattened nose, a flap of skin was cut out on a feeding pedicle (Fig. 1), which was moved to the refreshed edges of the nasal defect and a nose was created from it, close in shape to the natural one. Good blood supply to the flap ensured its engraftment. The disadvantage of the Indian method was that the extensive wound surface on the forehead after moving the flap was replaced by a disfiguring scar.
A further improvement of the Indian method of Rhinoplasty was the method proposed in 1845 by I. Dieffenbach. It consisted in cutting out a piece of skin from the forehead somewhat longer and, when suturing it to the edges of the defect, duplicating it along the edges of the wings. That. the skin lining of the wound surface of the flap was created, facing the nasal cavity within its wings. This modification contributed to less shrinkage of the flap and improved the shape of the nose, but a frequent complication was necrosis of the flap in the area of the inner lining (duplication). Subsequent modifications of the Indian method consisted in the fact that the flap was cut out not along the midline of the forehead, but from its lateral areas.
Rice. 2. Stage of rhinoplasty according to Shimanovsky (modification of the Indian method): a “support” for the nose is formed from soft tissues from the forehead area.
Yu. K. Shimanovsky in 1865 proposed creating a “support” to prevent retraction of the nasal bridge during subsequent plastic surgery. For this purpose, he cut out two symmetrical flaps of skin on both sides of the midline of the forehead with feeding legs at the eyebrows, lowered these flaps and installed them vertically along the midline of the pear-shaped aperture. Their wound surfaces were in close contact as a result of the application of mattress sutures and, thus, a support was created for the nose being formed (Fig. 2). However, this method did not eliminate the retraction of the back of the formed nose.
Another direction in the development of R. was the so-called. French or ancient Indian method, in which the skin of the cheeks was used to form the nose. The first such attempt was made by K. A. Hueter, who cut out two trapezoidal flaps from the areas of the cheeks adjacent to the pyriform aperture (the legs of these flaps were located at the medial corners of the eyes at the level of the root of the nose, and the apices were at the level of the bottom of the lower nasal moves), separated them and moved them to the existing defect. The inner edges of these flaps were sewn together, and the outer ones were sewn into the edges of the remaining strips of skin delimiting the edges of the pear-shaped aperture. On one of the flaps at the inner edge of the apex, he additionally cut out an additional strip of skin, from which he formed the nasal septum. No matter how widely the skin of the cheeks was separated, the required amount of material was still not enough to form the nose; the nose turned out to be short and flat and, in addition, scarring of the wound surface of the flaps facing the nasal cavity led to rough wrinkling of them, the shape of the nose was distorted. R.'s methods for complete defects of the nose from nearby tissues from the cheeks have not received further distribution.
Further attempts to create a stable, proportional shape of the nose with a bilateral epithelial lining came down to a combination of several R. methods and consisted in the fact that to form the internal epithelial lining of the nose, pedunculated flaps from the skin surrounding the defect were used, and for the outer coverings they borrowed skin from the forehead or from the periphery. As a result of such combinations, a nose of a more stable shape was obtained, but due to the lack of osteochondral support, its back sagged, the wings spread out, and the nose took on a flattened shape.
Another method of R., in which a flap of skin from the shoulder was used to form the nose, was the Italian method proposed by A. Branca in the mid-15th century. The operation he proposed was that on the shoulder in the area of the biceps muscle, two longitudinal incisions were made around a flap of skin of the required size, prepared and a piece of canvas was placed under it. After 10 days, one of the legs of the flap was cut off, the edges of the nasal defect were refreshed, the end of the flap was sutured to these edges, and the arm was bandaged to the head for 14 days. The flap was then cut freehand and the nasal wings and septum were formed. This method initially gained many supporters, but then gradually it began to be forgotten and for a long time was not used at all.
The disadvantages of the Italian method were frequent necrosis of the end of the flap due to insufficient nutrition and the long, painful forced position of the patient with his hand bandaged to the head, the difference in the color of the skin of the hand and face, as well as wrinkling of the flap as a result of scarring.
At the beginning of the 19th century. the Italian method with certain changes under the name of the New Italian method was revived in England by Lynn (1803) and J. S. Carpue (1814), and in Germany by S. F. Graefe (1816), which shortened the time required for the formation of a skin flap on the shoulder by suturing it directly to the exposed edges of the defect.
Rice. 3. Stage of the osteoplastic method of rhinoplasty according to Dyakonov (modification of the Indian method): formation of a skin-periosteal-bone flap from the forehead to form a “support” for the nose.
To eliminate the retraction of the nasal bridge, osteoplastic methods have been proposed. In 1859, B. Langenbeck developed a method of R. using a cutaneous periosteal flap from the forehead. This resulted in a denser and better shaped nose. At the same time, B. Langenbeck suggested the possibility of using a skin-periosteal-bone flap from the forehead, which was carried out in 1886 by F. Koenig and in 1891 by P. I. Dyakonov (Fig. 3). Total R. according to this principle was first produced in 1895 by K. Schimmelbusch.
In 1903, N.I. Napalkov proposed and successfully carried out a free transplantation of the mucous membrane for the internal lining of the nose. For this purpose, he used a free flap of the vaginal mucosa from a woman, the cut was made by R.; With this flap he covered the wound surface of the skin-periosteal-bone flap, cut from the forehead according to the Schimmelbusch method.
Rice. 4. Stage of rhinoplasty according to Israel (modification of the Italian method): a skin-periosteal-bone flap on a feeding pedicle, cut from the forearm along the ulna, is sutured to the upper edge of the nasal defect. Rice. 5. Stages of rhinoplasty according to Steinthal (modification of the Italian method): a - a migrating skin-periosteal flap from the anterior surface of the chest is sewn into the incision on the surface of the left forearm; b — the distal end of the flap is sutured to the upper edge of the nasal defect.
The technique of borrowing tissue from the periphery for R.'s purposes was improved and increasingly introduced into practice. In 1896, J. Israel proposed cutting out a cutaneous-periosteal-osseous flap to create a more permanent shape of the nose from the forearm along the ulna (Fig. 4). Steinthal (1901) was the first to use a migrating complex skin-periosteal flap from the anterior surface of the chest (Fig. 5) with pieces of costal cartilage to give stability to the nose and preserve the shape of its wings.
J. Israel's proposal (1896) to transplant free bone grafts under the skin of the deformed dorsum of the nose became widespread. In this case, a bone plate was crushed from the anterior edge of the tibia and, through an incision along the midline of the back of the nose, its upper end was brought to the exposed edge of the nasal part of the frontal bone and to the nasal bones; the lower end reached the top of the nose. In 1898, A. A. Ab-razhanov used for this purpose a plate of ox bone, pre-treated with ether and boiled in a 2% soda solution.
In 1900, P.I. Dyakonov modified Israel’s operation by making a skin incision not along the back of the nose, but across it in the area of the bridge of the nose. This significantly improved the cosmetic effect of the operation. In addition, he proposed a special knife, curved at an angle with a double-edged blade, which easily peeled off the tissue of the sunken bridge of the nose.
In 1906, Joseph (J. Joseph) developed an endonasal method of introducing a bone graft under the sunken soft tissue of the nasal dorsum. For this purpose, he made an incision under the edge of the lateral cartilage from the side of the nasal cavity.
In 1910, E. Lexer proposed a method of total R., which consisted in the fact that first a triangular plate, reminiscent in shape of the slopes of the dorsum of the nose, was cut out from the anterior edge of the tibia; this plate was placed under the skin of the shoulder or forearm. For this purpose, two parallel incisions were made and a bone plate was placed under the detached strip of skin. The edges of the skin were folded inward, etc. the bone graft was wrapped in skin on all sides. After three months, the edges of the defect were freshened, the corresponding end of the flap was cut off and sewn into the edges of the nasal defect. Wedge, observations have shown that a bone graft placed under the skin of the dorsum of the nose, without experiencing functional load, gradually resolves.
Methods using complex skin-periosteal-bone flaps formed from fingers or toes, developed by Hardie (J. Hardie, 1874), Kashchev (1897), R. R. Vreden (1902), N. M. Volkovich (1908) , led in some cases to deformities. These methods have not found application.
Subsequently, to preserve the shape of the nose, they began to use supporting prostheses, removable and permanent, inserted under the thickness of the preserved but deformed soft tissues of the nose. However, most of these prostheses at different times from the moment of surgery caused pressure sores of the skin or mucous membrane, the formation of fistulas, so they had to be removed. There is evidence of favorable and lasting results after inserting inserts made of polymeric materials under the soft tissue of the dorsum of the nose.
Photos "Before" and "After"
A YEAR AFTER CONSERVATING RHINOPLASTY
See more “Before” and “After” photos
The following techniques are used when performing the operation
- In closed rhinoplasty, incisions are made in the nostrils.
- In open rhinoplasty, an additional small incision is made through the columella, the tissue bridge between the nostrils.
- Both techniques gently mobilize the soft tissue covering the nose. Next, we work with cartilage and bone tissue to obtain the desired shape and size of the nose. If necessary, cartilage tissue is taken from the nasal septum, or in cases of revision, cartilage from the ear or rib may be required. If nasal breathing is difficult, septoplasty is performed to improve breathing. The fabrics are then re-draped and covered. The operation usually lasts two to three hours.
⇒ INFORMATION: How to get rid of a hump on the nose?
Indications and contraindications
Indications for rhinoplasty are associated with the following shape imperfections:
- Hump.
- Sharp or thick, hooked tip.
- Long length.
- Wide nostrils.
- Saddle shape.
Rhinoplasty is indicated for cases of deviated nasal septum and deformities, both congenital and resulting from trauma. The operation is performed in case of disturbance and complete cessation of nasal breathing.
The surgeon will refuse to perform the correction if the client:
- Diseases of the heart and blood vessels,
- Bleeding disorders;
- Diseases of the liver, kidneys;
- Diabetes;
- Active form of tuberculosis;
- Pregnancy, menstruation;
- Folliculitis (inflammation of the hair follicle), acne at the site of upcoming surgery;
- Acute viral infections;
- Cancer diseases;
- Mental disorders.
There are also age restrictions. Rhinoplasty is not performed until the age of 18 in girls and until the age of 21–23 in boys , which is associated with the process of formation of the facial part of the skull.
Correction is not recommended after 40 years of age, due to slower tissue regeneration and the risk of complications at this age. Older patients have a hard time getting used to a new look and often regret the changes.
During the consultation before the procedure, the surgeon finds out why the patient is interested in rhinoplasty, what result he expects, explains the consequences and warns about possible complications.
What is conservation rhinoplasty?
In most cases, when patients contact a plastic surgeon for rhinoplasty, the number one problem is the presence of a nasal hump . Therefore, reducing the nasal hump is an important surgical step in rhinoplasty. In classical rhinoplasty, after reducing the height of the dorsum, the nasal arch is destroyed and must be reconstructed. For the past few years, this technique has been a standard procedure used by surgeons to remove the hump and reshape the nose. The bony hump was removed using an osteotome and hammer and then removed, resulting in an open roof of the nasal dorsum, which had to be reconstructed using cartilage grafts and sutures.
Think of the nose as a multi-story building with the top floor being the hump. In standard rhinoplasty, the surgeon removes the top floor or hump to reduce the size of the building. This method leaves the roof exposed, which will then need to be repaired.
⇒ INFORMATION: Open and closed rhinoplasty: differences and features
What is nasal tip rhinoplasty?
Rhinoplasty of the tip of the nose is a partial correction of the shape of the nose, affecting only this part. The surgeon may recommend it as more gentle. This operation is indicated for patients whose nasal tip is irregularly shaped from birth, for example, teardrop-shaped, forked, hooked, curved from birth, disproportionately wide, has too wide, or less often too narrow nostrils. You can also change the angle of your nose. For a plastic surgeon, this is jewelry work; every millimeter is important. As in other cases, the patient’s initial anatomy, the condition of the cartilage and the thickness of the skin play a big role.
As follows from the above, with this method of correction, problems with a hump on the back of the nose cannot be solved. This will require more thorough intervention. The advantages include the possibility of local anesthesia.
Benefits of conservation rhinoplasty
- With the Preservation Rhinoplasty technique, there is no need to destroy or reconstruct the back or roof during surgery . The height is changed by removing the lower floors of the building in this design, so the nose becomes smaller, the hump disappears, and the roof of the upper floor remains intact.
- With this approach, the bridge of the nose remains natural. The bones and cartilaginous structures that form the bridge of the nose are preserved. Excess cartilage and bone fragments are removed only from certain areas of the nose, allowing the bridge of the nose to be pressed inward. Thus, the normal anatomy of the bony part of the back is preserved and a natural result is achieved without traces of aesthetic surgery.
- Light and shadow reflected from the bridge maintain attractive lines and provide a natural bridge to the nose.
- Conserving rhinoplasty poses a lower risk of breathing problems after surgery. In traditional rhinoplasty, some of the functional structures of the nose that are essential for proper breathing are destroyed and need to be reconstructed.
- Incomplete or incorrect reconstruction during traditional rhinoplasty can lead to long-term breathing problems. Conservative rhinoplasty preserves these nasal structures so that there is no need for reconstruction during surgery.
- An additional feature of conservation rhinoplasty is that it is performed in a different plane of dissection than traditional rhinoplasty. Dissection is carried out in the subperichondrial and subperiosteal planes. The significance of this is that the soft tissues of the nose (which carry blood vessels and lymph nodes) are not damaged or destroyed. Maintaining intact blood vessels and lymph nodes results in minimal swelling and bruising, resulting in a significantly faster recovery than traditional rhinoplasty.
- With conservation rhinoplasty, the risk of bleeding after surgery is reduced, meaning that air ducts inserted into the nose allow the patient to breathe immediately.
- This technique is less invasive and traumatic for the patient. Preserving the back, while promoting a more natural-looking result, also avoids secondary deformities that sometimes lead to the need for revision surgery.
- The rehabilitation period is faster and patients can quickly return to their normal lifestyle.
⇒ INFORMATION: Medical indications for correcting the shape of the nose
Operation video
To make it clear how nose rhinoplasty is done, we suggest watching a video of the operation.
Non-surgical rhinoplasty
They resort to it if small defects need to be eliminated. Performed in 5–7% of patients.
To smooth or change the angles of the tip of the nose, restore symmetry, and disguise the hump, fillers are used. The disadvantage of this correction is that after 12–18 months the fillers dissolve, leaving the risk of migration of the substance.
Absorbable drugs are also used. This way you can get rid of unevenness and bulges. The technique is used on the tip, wings, supra-tip zone, and occasionally on the hump. It takes place in several stages.
Aptos threads, which are inserted through punctures, allow you to tighten the tip and correct the shape of the wings. This technique is unpopular because there is a risk of thread breaking and rough scars appearing.
Piezorrhinoplasty
Piezo is a system that converts electrical energy into ultrasound, allowing the surgeon to truly “sculpt” the nasal bones, changing their shape and thickness as needed, and even trimming them if necessary, without causing problems to other sensitive tissues of the nose.
Piezo uses ultrasonic vibrations at a frequency of 25-29 kHz to change the shape of bone, while leaving all soft tissues affected by frequencies above 50 kHz, such as skin, mucous membranes, blood vessels and nerves, completely intact.
Piezo technology has been known for several years and is mainly used in dentistry with excellent results in the treatment of the upper and lower jaw.
In traditional rhinoplasty, surgical instruments known as rasps and osteotomes (hammer and chisel) are used to reshape the nasal bones by removing the hump and narrowing the width of the nasal bone. These tools are relatively imprecise and their use can result in uneven contours if not used properly.
Recently, a technology has been developed that uses ultrasonic waves to precisely influence bone tissue and is much less traumatic compared to traditional methods.
Ultrasound or piezo rhinoplasty is currently the most advanced technique available for minimally traumatic nasal bone reshaping and hump removal during rhinoplasty.
The ultrasound rhinoplasty technique differs from the traditional one.
- A complete detachment of the soft tissue over the bony surface is required, allowing the entire architecture of the nasal bone to be seen.
- The ultrasonic pen can be equipped with a variety of tips that can remove hump, polish any rough surfaces, make precise bone cuts that do not damage the underlying mucosa.
As a result, an attractive aesthetic result can be achieved with much less trauma, less swelling and almost no bruising.
⇒ INFORMATION: What absolutely should not be done after rhinoplasty
Benefits of piezorhinoplasty
- Reducing the level of soft tissue trauma to a minimum. Therefore, bruising and swelling are practically absent.
- Controlled cuts create clean, even lines.
- Prevents uncontrolled bone fractures unlike osteotomy techniques. Thus, it prevents deformations and unevenness.
- Post-operative recovery is faster because it does not cause damage to soft tissue, surrounding blood vessels and cartilage, so patients can return to their daily lives more quickly. Postoperative pain is also usually less.
- The accuracy of reshaping the nasal bones is higher, which leads to increased patient satisfaction.
- The incidence of complications after rhinoplasty and the need for revision surgery is reduced.
Complications during rhinoplasty
Any surgical operation can cause complications, because only the surgeon who does not operate makes no mistakes. Knowledge about possible complications and consequences is necessary to make the right decision, reduce the number of such cases, minimize their severity and treat them if they occur. Some complications of rhinoplasty are related to anesthesia and are not covered in this article. Anaphylactic reactions to general or local anesthesia call into question the knowledge and skills of the anesthesiologist, surgeon and assistants.
Complications of rhinoplasty
can be divided into 4 categories:
- Occurring during surgery;
- Occurring immediately after surgery;
- Ambulances;
- Postponed.
What is a complication?
In general, a complication can be described as an unexpected occurrence during or after surgery of a medical or surgical circumstance that requires special attention. Such cases are easy to recognize, but aesthetic complications are much more difficult to identify, because they are based on the surgeon’s vision and the patient’s ideas about his body. The last factor can take different forms:
- The patient’s appearance:
how do others see him? In society there are certain standards of beauty and unattractiveness. By transferring these standards to oneself, the patient may feel vulnerable; - The patient’s perception of reality:
how does he see himself? Does this feeling match how others see him? - The degree of importance a patient places on their appearance:
Some may not think about it at all, while others attach great importance to appearance. - The patient's degree of satisfaction with his appearance:
dissatisfaction can range from mild dissatisfaction and concern to dysmorphic disorders leading to obsessive states. Approximately 2% of plastic surgery clients require evaluation by a psychiatrist.
Aesthetic perception is difficult to define, so the result of the operation is always unpredictable. It depends on modern fashion, media influence, cultural and ethnic characteristics.
From a practical point of view, the beauty of the nose is based on three indicators: the ratio of the width and height of the frontal, transverse and basal defects. Based on this, a three-dimensional model of the nose is created. Purpose of rhinoplasty
– improve the existing harmony without disturbing the functional structure.
Complication rate
According to data recorded in the literature, the number of complications during nasal surgery reaches 4-18.8%. For each individual surgeon, this figure decreases with the accumulation of experience. Complications related to the skin and soft tissues occur in 10% of cases. On average, severe systemic or life-threatening consequences occur after 1.7-5% of operations. Intracranial complications are extremely rare.
Description
Clinical manifestations of rhinoplasty complications can be classified as follows:
- Functional;
- Infectious;
- Aesthetic;
- Psychological
; - Specific.
Complications during surgery
Excessive bleeding
. This may be a consequence of congenital or acquired coagulopathy. Such circumstances must be identified before surgery. If excessive bleeding occurs unexpectedly, urgent consultation with a hematologist is required. As a rule, acquired coagulopathy is triggered by taking medications, most often aspirin. Its use should be stopped 2 weeks before surgery.
The main cause of excessive bleeding is fibrinolysis. This occurs due to abnormal activation of the fibrinolytic system, as a result of which the clotted blood is instantly resorbed. Diagnosis requires tests for the content of fibrinogen and its breakdown products in the blood. To stop bleeding, blood products, norleucine and tranexamic acid are used. However, these substances can cause deep vein thrombosis and pulmonary embolism.
Also, excessive bleeding during surgery can result from blood stagnation, making the surgeon's job more difficult. This happens in 0.3-1% of cases.
Ruptures of mucocartilaginous flaps
. Patient and careful operation usually avoids such complications, however, they can occur if the nose has previously been injured or operated on.
Unilateral tears will heal on their own, but bilateral symmetrical tears can lead to septal perforation and subsequent complications. Such gaps are closed immediately during surgery. Improper closure can lead to adhesions and nasal obstruction, requiring subsequent surgery.
Skin tear
.
This complication is possible when the skin is cut, especially in the area of the nasal arch. The surgeon can avoid this only by being extremely careful. Tearing the skin will cause scarring
, so sutures should be applied with minimal tension. If a scar does appear, further therapy may be needed.
Burns
. May occur due to equipment malfunctions or surgeon error. Therefore, special care is required when using cauterization tools. When a burn occurs, various measures are taken depending on the circumstances. Skin necrosis will result in scar formation.
Destruction of the bone pyramid
. Fracture may occur when the bony tubercle is removed using an osteotome, especially if the patient has a history of nasal trauma or the vomer (the flat, trapezoid-shaped bone that forms the back of the nasal septum) or ethmoid bone has been injured in previous surgery. In such cases, filing with a rasp is recommended.
Repair requires careful positioning of the fragments and provision of constant internal and external fixation during healing.
Disarticulation of the superior transverse cartilage
. This complication can occur when cutting bone with a rasp. Bilateral disarticulation creates an inverted V-shaped deformity, while unilateral disarticulation leads to asymmetry in the middle third of the nose. Applying tissue flaps will eliminate venting symptoms and aesthetic deficiencies.
Complications after osteotomy
. "Depression". This deformity is a consequence of a fracture in the upper thick part of the bone of the frontonasal junction. Attempting to narrow the transected bone will result in lateralization of the superior segment. The fracture needs to be moved lower along the nasal bone.
- "Open Roof" If the side segments do not meet the bridge of the nose, the resulting gap will become visible and palpable to the touch. If left unattended, the mucous membrane will adhere to the overhanging soft tissue and create pressure. Correction involves centering the bridge of the nose and aligning the lateral segments.
The cause of an “open roof” may be:
- Fracture of the cranial bone during osteotomy;
- Inability to center debris;
- Excessive seals in the nose.
- "Step" deformation. It is formed when a unilateral osteotomy is performed too far from the middle of the nasofacial groove, then a visible hump is formed on the side of the nose. Correction involves repeat osteotomy.
Perinasal injury
. During osteotomy, especially on previously injured noses, there is a high probability of recurrence of old fractures. These bones are very susceptible to external influences. A surgeon’s mistake can have an immediate impact, or it can manifest itself in the form of a subsequent infection. Orbital hemorrhage or panniculitis is a threat to vision and requires immediate medical attention. Injuries to the nasolacrimal system are also likely, in which case it may be necessary to open a pocket in the nasal cavity. There have also been cases of damage to the infraorbital nerve. Complications associated with skull injury are described below.
Complications that occur immediately after surgery
Obstacles to breathing
. Suctioning blood after extubation may cause laryngeal spasm. In this case, medications that induce muscle relaxation, reintubation, or ventilation may be necessary. Nasal packs or splints can also obstruct breathing. Therefore, special care must be taken when placing them.
Anaphylaxis
. Anaphylaxis is a possibility when antibiotics are used during surgery. Cases of anaphylactic shock have been reported from bacitracin and latex tampons.
Deterioration of vision
. After injection of local anesthetics and vasoconstrictors, temporary or permanent visual impairment may occur. The reason for this may be vasospasm or thromboembolism, causing ocular ischemia. If symptoms persist, you should consult a doctor.
Immediate complications
Bleeding
. Complications (rhinoplasty rarely causes them) occur in 2-4% of cases. As a rule, the source of bleeding is localized using vasoconstrictors. It is also possible to cauterize the torn vessel. Antibiotic swabs and dressings may be needed.
Septal hematoma
. Daily suction will be needed to clear the passage of blood. Some specialists resort to incision and installation of a drainage device. To avoid an abscess in the septum, antibiotics are used.
Infections
- Infections in the wound. Such complications after rhinoplasty occur only in 2% of cases. Localized panniculitis, abscess, or granuloma is treated with antibiotics or drainage. Infection can also be caused by the use of foreign materials.
- Sepsis. It is important to be aware of the dangers of this complication after rhinoplasty. Exacerbation of infection can lead to acute insufficiency of blood supply and multiple organ dysfunctions. Treatments include antibiotics, hormones, and therapy for insufficiency of the circulatory system.
- Toxic shock syndrome. Postoperative fever, vomiting, diarrhea, low blood pressure without obvious blood loss, and an erythematous rash are signs of this syndrome. In severe cases, the condition may worsen. After a few days, peeling of the palms and soles begins. Toxic shock syndrome toxin-1, produced by Staphylococcus aureus bacteria, is the cause of the disease. Carriers of these bacteria are 18-50% of the healthy population.
Measures taken during treatment:
- Removing nasal swabs, cleaning the bacterial environment;
- Taking antibiotics;
- Examination of the body;
- Aggressive therapy of the circulatory system.
Toxic shock syndrome during nasal surgery occurs in 0.016% of cases, with a mortality rate of 11%.
- Subacute bacterial endocarditis. Every patient with a heart murmur is at risk. It is necessary to monitor your oral health and take antibiotics for prevention. If such a complication occurs, blood tests are needed.
- Intracranial infections. The proximity of the edges of the cranial bone and traumatic manipulations during rhinoplasty
increase the likelihood of meningitis, subdural empyema, and intracranial abscesses. If you experience symptoms such as headaches, lethargy, high fever, twitching of the cranial nerves, you should consult a doctor. - Acute and/or chronic sinusitis. It may be a consequence of rhinoplasty and requires endoscopic surgery.
Seam divergence
.
Usually this goes unnoticed. Adhesions may form, but they too will gradually heal. But if the through incision diverges, urgent intervention is required, otherwise a scar
.
Persistent swelling
. Effects of rhinoplasty may include initial swelling and periorbital bruising that lasts up to 10 days. The severity of swelling after rhinoplasty depends on the complexity of the osteotomy, the instruments used, the length of the operation, excessive use of tampons, postoperative vomiting, or high blood pressure. To avoid all of the above and prevent swelling after rhinoplasty, a bandage is applied immediately after the osteotomy, dexamethasone is administered intravenously during the operation, after the operation the head should be kept in an elevated position, a cold compress should be applied to the nose, and blood pressure should be constantly monitored. Persistent swelling and numbness of the tip of the nose are possible with external rhinoplasty. Swelling after rhinoplasty can last up to several months.
Dead skin
.
Excessive damage and unreasonable use of cauterization apparatus can lead to skin death. The consequences of rhinoplasty cause poor blood supply and infection. A bandage applied too tightly can lead to the same result. In case of necrosis, sanitation and re-healing are necessary. Subsequently, to get rid of the scar, local hormonal injections, dermabrasion
, laser resurfacing and even surgical reconstruction are used.
Necrosis of part of the bone
. Necrosis of bone or cartilage may occur, followed by infection, displacement, or associated impairment (aesthetic or functional). In such cases, the infection is first controlled with antibiotics and then debridement is performed. Reconstructive surgery may be needed in the future.
Cardiovascular failure. In elderly patients and patients with heart disease, nasal packing may cause hypoxia. In such cases, oxygen therapy is recommended.
Nasal liquorrhea
. The frequency of such complications is extremely low. Most often, liquorrhea is caused by previous injuries or the presence of congenital bone defects. Most leaks heal on their own. If this does not happen, intra- and extracranial surgical techniques are used.
Contact dermatitis
Allergy
occurs in patients with high sensitivity as a reaction to applied bandages. Treatment involves removing them and taking antihistamines or hormonal drugs.
Blockage of the nasal passages
. The swelling that occurs after surgery can lead to permanent nasal blockage. This condition is usually associated with vasomotor rhinopathy or allergic rhinitis. Those who do not respond to drug treatment will need surgery.
Numbness and pain
. Persistent numbness and pain behind the upper incisors may be due to neurapaxia of the nasopalatine nerve.
Smell disorders
. A short-term decrease in the sense of smell immediately after surgery is quite reasonable and can have several causes, for example, swelling, damage to the neuroepithelium, or the use of certain medications.
Patients with previous facial trauma may be predisposed to injury to the olfactory system during osteotomy. Neurotrophic viral infections, as well as psychogenic factors, can cause surgical intervention. Complete loss of smell is observed in 1% of cases.
Carotid-cavernous fistula
.
This is a rare post-traumatic complication. Constant fluctuations in pressure in the fistula cause eye pain, proptosis (pathological displacement of an organ or part of it forward), ophthalmoplegia (paralysis of the eye muscles due to damage to the oculomotor nerves), blurred vision and noise. These symptoms indicate a diagnosis that can be confirmed by angiography (contrast X-ray examination of blood vessels
).
Confirmation requirement
. Some patients require constant confirmation from the surgeon that the blockage of the nasal passages will pass, the senses of taste and smell will return, the tip of the nose will change its position, and the swelling will subside.
Early psychological complications
. It is not uncommon for patients to experience short-term episodes of anxiety or depression that can last up to 6 weeks.
Delayed complications
Hypertrophic scars
.
They can ruin the result of any brilliantly performed rhinoplasty. Losing skin due to infection or death becomes a real disaster. It is necessary to try to reduce the size of the scar using hormonal injections. Next, dermabrasion, lasers
, and surgery are used.
Beak-shaped nose deformity . This type of deformity involves drooping of the tip of the nose. The reason lies in the incorrect correction of the cartilaginous back or septum of the nose (hard beak) or in the accumulation of excess tissue during the formation of a scar (soft beak). The correction consists of reducing the cartilaginous back and septum and/or cutting off the soft tissue.
Formation of adhesions. The formation of adhesions or adhesion occurs when two hard surfaces come into contact. Stenting is used to prevent it. Endoscopic dissection is used to eliminate it.
Perforation of the septum . This complication can occur in 3-24.5% of cases. For small holes, surgical closure may be used. In general, there are many methods and techniques of execution. If none of them brings results, use partition buttons.
Destruction of the nasal valve. This complication is a consequence of an overly aggressive cutting technique of the transverse cartilage. Damage to the valve will cause breathing difficulties.
Narrowing of the nasal passages. This is an extremely serious complication, and it is associated with the cutting off of excess tissue from the inside of the nostril. The narrowing makes breathing difficult and causes constant discomfort. Reconstructive surgery can correct the situation.
Formation of bulges . As a rule, they form at the tip of the nose in 2% of cases. While bilateral symmetrical bumps may be aesthetically pleasing, a bump on one side of the nose requires surgery. Therefore, during rhinoplasty, it is necessary to ensure the absolute symmetry and equality of the remnants of the transverse cartilage. Most often, bulges are formed due to lack of symmetry, the use of destructive rhinoplasty techniques, thin skin, or the formation of too large scars.
Recurrent meningitis. Constant attacks of meningitis may be a consequence of the inability to identify a hidden fistula. In addition to stopping the meningitis itself, you need to look for its cause.
Osteogranuloma. Non-absorbable fatty materials used during surgery can provoke an inflammatory process (called oleogranuloma, paraffinoma, oil granuloma, sclerosing lipogranulomatosis). Other causes should be excluded using computed tomography. In case of surgical intervention, relapse is possible.
Cyst of the nasal dorsum. The nasal mucosa, which has shifted to the subcutaneous layers, leads to this rare complication. Surgery is possible.
Aesthetically unsatisfactory result. Insufficient or excessive correction of nasal imperfections leads either to the preservation of an existing defect or to the formation of a new one. In the latter case, functional impairment may also occur. Some newly formed defects are only apparent and are corrected only after an accurate diagnosis has been made. In general, revision rhinoplasty should not be performed within 12 months of the first surgery.
Such defects can occur together or individually and usually affect the width, height or depth of various parts of the nose.
Upper third defects
- Deep nasolabial cavity. Various implants
and flaps are used for correction. - Small nasolabial depression. Deepening can be done by removing the procerus muscle. If the cause lies in the bone, then osteotomy or partial removal is used.
- Expansion of the upper third. The cause may be improper medialization of the nasal bones after osteotomy or fractures of the skull bones. Correction includes septal realignment and re-osteotomy.
- Convexity of the upper third. Correction involves reducing the defect, usually by filing.
- Excessive reduction of the upper third. The resulting depression needs to be corrected. If part of the septum is missing, it needs to be restored.
- Asymmetry of the upper third. Causes may include uneven nasal bone remnants, asymmetrical healing, or deviated septum.
Middle third defects
- Expansion of the middle third. It is usually the result of fusion of bone and cartilage and subsequent widening of the upper third of the nose. However, this defect may only be visible if there is drooping of the tip of the nose.
- Convexity of the middle third. As a rule, this is a consequence of a beak-shaped nose deformation. Correction is made by removing excess cartilage or soft tissue.
- Depression in the middle third. The septum is built up and, if necessary, restored.
- Asymmetry of the middle third. The reason may lie in unequal bone remnants, unilateral displacement of cartilage, and asymmetric healing.
Defects of the lower third
- Widening and convexity of the lower third. This occurs when the base of the lower part of the cartilage is destroyed.
- Wide or square nose tip.
- Narrow or small tip of the nose. The reason may be the destruction of the end of the cartilage. In addition, lump formation or destruction of the nasal valve may occur. The tip of the nose is restored using flap techniques. Breathing problems are addressed separately.
- Asymmetrical tip of the nose. May be the result of destruction of the cartilage structure. Correction depends on the cause. Flap techniques can be used.
- Protruding tip of the nose.
- Wide septum of the nasal vestibule. As a rule, this is an initial defect that is not corrected during rhinoplasty. Excess soft tissue is removed from the septum.
- Hanging septum of the nasal vestibule. The cause may be deeply located “legs” of the septum, their removal and subsequent scar formation. The method of correction depends on the cause.
- Drooping nostrils. The cause may be excessive cutting off of the legs of the septum. Correction is made only after an accurate diagnosis has been made.
- Holes in the wings of the nose. Excessive removal of the lateral legs of the septum deprives the nostrils of support, as a result of which they collapse and make breathing difficult.
- Asymmetry of the nostrils. The cause may be the septum of the vestibule of the nose or its wings.
- Retracted nasolabial cavity. The cause may be excessive removal of the base of the septal cartilage. Flaps are used for correction.
- Long nasolabial cavity. This defect may be apparent due to the raised tip of the nose. Otherwise, it is possible to remove excess soft tissue or correct the bridge of the nose.
Others
- Flap/implant migration. Such complications include resorption, movement or rejection of the implanted material. Allogeneic transplants are much more prone to rejection and infection. And if antibiotics do not help, the implant is removed, after which the correction is carried out again.
- Disproportional nose. It looks inharmonious and is a consequence of the mediocre work of the surgeon. After assessing the current situation, reconstructive rhinoplasty is performed.
- Maxillofacial defects. A brilliant rhinoplasty can be ruined if existing maxillofacial defects go unnoticed before surgery. All components of both jaws, lips and the condition of the teeth should be examined in advance.
Revision rhinoplasty is required in 5-15% of cases. Any correction operations are carried out with the possibility of requiring further corrections.
Persistent psychological complications
.
Many studies have been conducted on this topic, the results of which are completely contradictory. Some argue that rhinoplasty patients have mental disorders and a predisposition to personality disorders. Others insist that such people do not show signs of mental pathology. Some studies even prove that after surgery people become calmer, their anxiety, hostility, paranoid syndromes disappear, and their self-esteem increases. Even patients with a shaky psyche receive a positive effect from rhinoplasty. However, for some, psychological balance
may still be disturbed.
Dental complications
. During surgery, the neurovascular system of the teeth may be damaged, which leads to the death of the pulp. Treatment should be carried out by a dentist.
Gustatory rhinorrhea
. Improper restoration of nerve tissue damaged during surgery leads to gustatory rhinorrhea. Treatment can be difficult, but antihistamines sometimes help.
Adjuvant disease
. This is an autoimmune disease caused by hypersensitivity to the implanted material. Often the cause may be a genetic predisposition. In some patients, symptoms can be relieved by removing the implants. Otherwise, contact a rheumatologist.
Lacrimal fistula
. Due to the proximity of the lacrimal drainage system to the site of the osteotomy, damage is possible. However, this happens extremely rarely.
Enophthalmos and silent fistula syndrome
. Such complications can be a consequence of septorhinoplasty.
Patient dissatisfaction
.
Aesthetic surgeries can have four outcomes:
- A satisfied patient means a satisfied surgeon;
- A satisfied patient means a dissatisfied surgeon;
- A dissatisfied patient is a satisfied surgeon;
- A dissatisfied patient means a dissatisfied surgeon.
The reason for the surgeon's dissatisfaction is most often his own perfectionism, but the patient's dissatisfaction can have many reasons, each of which is unique. The surgeon must carefully select patients and examine their psychological status.
No surgical operation is immune from complications. This obliges the surgeon to be prepared for them, to know preventive measures and correction techniques. Patients should also be informed about possible complications in order to weigh all possible risks before surgery.
The surgeon minimizes complications through careful selection of patients (both from a medical and psychological point of view), establishing the type of defect and selecting a correction method.
Future of Operation
With an increasing understanding of the anatomical, psychological and pathological factors involved in the aesthetic and functional aspects of rhinoplasty, techniques will become more accurate and the number of complications will decrease. Aesthetic trends that society dictates to us will also influence the operation. Implantation materials will become safer for patients, simpler for surgeons, and will also become more effective at restoring volume while causing minimal complications. And technological innovations in the field of endoscopic rhinoplasty and computer diagnostics will greatly facilitate the choice of one or another correction technique.
How to prepare for rhinoplasty
- Avoid taking medications containing aspirin or ibuprofen for two weeks before and after surgery. These medications may increase the risk of bleeding.
- Also avoid herbal remedies and dietary supplements. If you smoke, reduce the number of cigarettes you smoke or quit smoking.
- Smoking slows down the healing process after surgery and may increase the chance of developing an infection.
- Plan to take 2 weeks off.
- After surgery, you will feel better every day during the first week.
- Bruising and swelling practically disappear 10-14 days after rhinoplasty.
Preparation
Nose correction takes place after preparation. Your surgeon will instruct you on how to prepare for rhinoplasty.
Preparation for rhinoplasty involves standard examinations:
- Electrocardiogram.
- Chest X-ray or fluorography.
- Picture of the nose.
2 weeks before the upcoming procedure, stop taking blood thinning medications . 7 days before rhinoplasty, it is recommended to refrain from drinking alcohol and smoking. Light food is left in the diet for 24 hours, and food and water are abandoned 6 hours before.
Before the operation, consultations with an anesthesiologist are held. The specialist clarifies information about anesthesia tolerance.
List of tests
The following tests are performed before rhinoplasty:
- Blood (general, biochemical, electrolytes, coagulogram, blood group, Rh factor), - within 14 days.
- HIV, HBS, HCV, RW - within 3 months.
- Urine - 14 days in advance.
Does it hurt?
During the rhinoplasty itself, the patient does not feel anything, because he is in a state of medicated sleep or the doctor applies an analgesic.
During the rehabilitation period, there is more inconvenience than pain - for example, due to tampons in the nose, which are removed after a day, and swelling. Compared to breast surgery, rhinoplasty is said to be painless.
Rules for successful rehabilitation after rhinoplasty
After rhinoplasty, you need to spend a day in the clinic. You should stay in bed with your head elevated above your chest to reduce bleeding and swelling. Some nosebleeds are possible for a few days. Special silicone air duct plates are placed in the nose, so patients can breathe through their nose immediately after surgery. Significant bruising and swelling around the eyes is normal and usually disappears within 7-10 days after surgery.
To further reduce the chance of bleeding and swelling, take precautions for several weeks after surgery.
Precautionary measures
- Avoid strenuous exercise such as aerobics and running.
- Don't blow your nose.
- Eat high-fiber foods such as fruits and vegetables to avoid constipation.
- Avoid extreme facial expressions such as smiling or laughing.
- Brush your teeth gently to limit movement of your upper lip.
- Wear clothes that button in the front. Do not place clothing such as shirts or sweaters over your head.
What are the risks of rhinoplasty?
We are talking about surgery, which is associated with risks, and sometimes side effects are observed. These are good reasons not to undergo rhinoplasty, especially if the surgeon does not see any abnormalities or medical indications.
An anaphylactic reaction to anesthesia is possible - a rapid allergy phenomenon that threatens life. In 0.017% of cases, toxic shock syndrome is observed - a shock condition that is caused by the activity of exotoxins from bacteria or viruses.
Overall, adverse events develop in only 4–18.8% of patients, with one in ten of this group experiencing skin and soft tissue complications.
During the operation, excessive bleeding, ruptures of the skin, mucocartilaginous structures, burns, violations of the bony pyramid, and others are recorded.
In the first hours and days after surgery, anaphylaxis and visual and respiratory dysfunction may develop. Hidden complications include bleeding and septal hematoma.
Very rarely , an infection gets into the wound, which requires a course of treatment with antibiotics; in the case of sepsis (blood poisoning), hormones and blood transfusions are used.
Other complications include:
- Decreased sensitivity.
- Scars, cicatrices requiring repeated intervention.
- Difficulty breathing.
- Deterioration of sense of smell.
- Perforation (holes) of the nasal septum.
- Cartilage atrophy.
- The appearance of a vascular network, pigmentation.
- Rarely - necrosis (death) of tissue.
In addition, the patient is not always satisfied with the result - 3 out of 10 such patients . The probability that the view will be as planned is about 70% . The nose may seem too regular, look unnatural, and may not fit in with the rest of your facial features. Therefore, before deciding to make changes, you should weigh the pros and cons.
After this, repeated correction may be required, which is carried out after 6 months, but not earlier. Indications include improperly stitched or excessively removed cartilage, in which the nose appears short, small columella (the lower part between the nasal passages), etc.
When is it better to refuse surgery?
People with dysmorphophobia or body dysmorphomania often turn to plastic surgeons for help. In the first case, we are talking about a painful attitude towards a minor defect or feature of the body, in the second - about an imaginary external defect.
If the surgeon does not find deviations from the average parameters in the size of the nose or its location in relation to other parts of the face, a consultation with a psychologist is recommended.
You should also study reviews about the clinic and the specific specialist. The lower the qualifications of the doctor, the higher the likelihood of complications.
↓
Early recovery period
- You will experience nasal swelling for several weeks, then your condition will gradually improve.
- Nasal breathing may also be impaired for a few weeks, but will improve as swelling decreases.
- For a short time after surgery, patients may experience swelling, nasal pain, or a dull headache.
- Most patients take pain medication for three to four days and return to work in just over a week after surgery.
- The results of rhinoplasty gradually become apparent as time passes and swelling decreases.
- Swelling may occur occasionally in the first year after the procedure. It is usually more noticeable in the morning and disappears throughout the day.
- Contact lenses can be worn immediately after rhinoplasty, but glasses should not be worn for several months after surgery.
Before surgery
Rhinoplasty is a full-fledged surgical procedure and is performed under general anesthesia in combination with local anesthesia. In this regard, the patient must undergo a comprehensive examination, including clinical and laboratory examination and consultation with specialists (ENT, therapist, anesthesiologist). To avoid complications during surgery, you should promptly notify the doctor about the presence of chronic and acute diseases at the time of the proposed surgical intervention, past illnesses, possible allergic reactions to medications, etc. Rhinoplasty is performed in a specialized clinic.
Rhinoplasty, like most plastic surgeries, imposes some temporary restrictions on lifestyle before the operation: it is undesirable to smoke, take aspirin and other drugs that affect blood clotting, because this can cause bleeding during surgery.